Endocrinology Specialist
Dr. Kashif Latif
Doctors have a variety of ways of finding their life's calling. For Kashif Latif, it was simply a matter of a disease hitting too close to home.
The Pakistani native arrived in the U.S. as a young student, intent on becoming a doctor. “Since my parents paid for my education, we had to succeed.
There was no option,” he explained with a smile. After attending Aga Khan University Medical College in Pakistan, Latif practiced internal medicine in Dyersburg, but when his then girlfriend, Shazia Hussain, received a fellowship to train at Le Bonheur Children's Medical Center, Latif followed suit. He came to Memphis in 1992 and completed a fellowship in internal medicine at the University of Tennessee. He and Hussain, a pediatrician with Pediatrics East, were married in 1997.
Latif practiced internal medicine until his son, Ahmed, was born. But at 11 months, the couple received a surprising diagnosis: Their child had juvenile diabetes. Learning how to monitor and live with this chronic disease illuminated a path for Latif.
“I learned a lot that I didn't appreciate before my son got diabetes,” he said. “Going through it day-to-day, having the disease under my roof made me realize that there's so much more than writing down a number and making a prescription.”
Soon, he returned to school to obtain a specialty in endocrinology and upon completing his training, opened AM Diabetes and Endocrinology Center in 2002. The center is named in honor of his son.
His son's diabetes made Latif aware of how important education is for patients, who are sometimes required to make significant lifestyle changes in order to manage their disease more effectively. His emphasis for the center is “to bring quality, comprehensive care for people with diabetes. The cornerstone for managing diabetes is education, so we've invested lots of resources into establishing a quality education center.”
It couldn't be in a better location. Because of the prevalence of obesity, poor eating habits, and a lack of exercise found across the Mid-South, diabetes is higher here than many other regions nationally.
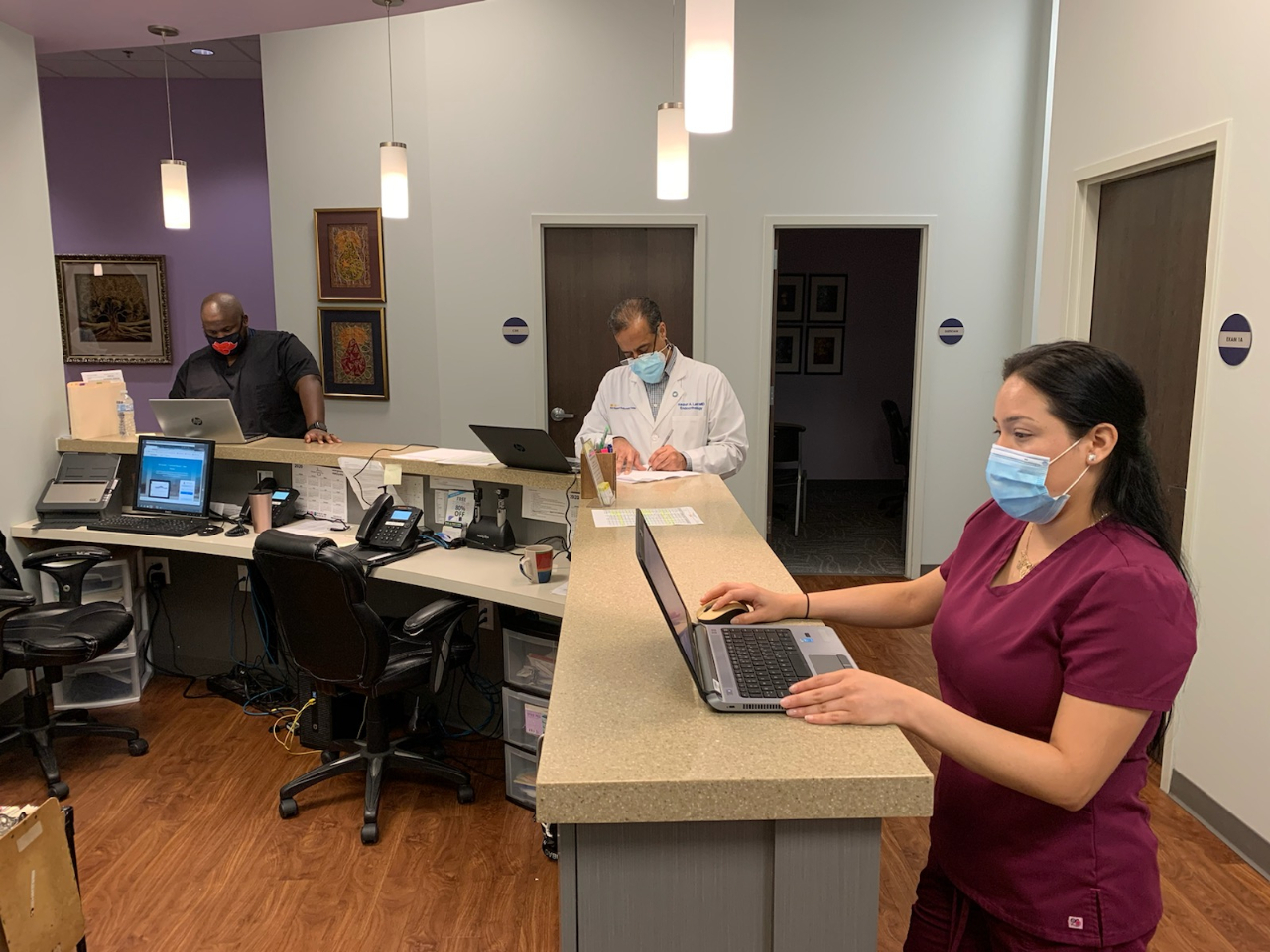
To address the problem head-on, Latif has built a staff of healthcare providers, including dieticians, physicians, and even a psychologist who help patients monitor the many complications that can arise with diabetes. They provide eye exams, cardiovascular check-ups, kidney function tests, blood work that monitors cholesterol and hemoglobin levels, and neurological checks. Latif's goal is to create a one-stop shop for diabetes treatment, not just for the patients he sees, but for those being referred by other physicians as well.
Latif's center has received certification from the American Diabetes Association, a rigorous process which requires clinics to closely document patient care. What Latif has discovered is that educating patients on diet, exercise, and lifestyle changes has enabled many of them to manage their diabetes with minimal medication. “For last three years we've had a positive impact for blood glucose control for those who attend the sessions,” he said. Yet despite that good news, insurance companies often don't want to reimburse for education.
And educating patients isn't easy, notes Latif. “There's push back from patients. When you use the word education, they say ‘We know what to eat. We know what to do.’” It can be a real problem. “But I tell patients, your diabetes is here and it's here to stay. The only way to make it go away is to turn back the hands of time.”
The education sessions patients receive takes eight hours, plus one follow-up three months later. Latif recommends most of his patients see an educator once a year, but does suggest some patients see his staff weekly “because they need to understand the disease process and how to control its impact.” Since diabetes is a long-term, chronic illness, patients must learn how to monitor their blood glucose levels and manage their diets to prevent serious complications.
To help patients with blood monitoring, Latif is using the latest in diabetes treatment technology: Professional Continuous Glucose Monitoring (CGM) therapy management and software. Latif's is also one of five clinics nationally, that, in addition to working with patients using CGM are also providing physician training in the use of the device.
As for life at home with a diabetic, Latif is quick to point out that his son receives no preferential treatment because of his illness. He routinely tells his son that diabetes is his test, and how well he does with it will be his report card. “He is still expected to perform in school and sports. There’s no specialty in our house, he doesn't get any privileges.” But what he does get is the excellent care of a father determined to make a difference in diabetes treatment.
A M Diabetes Center/ Insulin Pump Center
What is the Insulin Pump Center?

Our experience in treatment of diabetes with insulin pumps has led to the creation of a comprehensive Insulin Pump Center (IPC) where patients with diabetes who are on insulin pumps are managed. This is the first of its kind in the nation. The Insulin Pump Center provides services from basic teaching about pump therapy to advanced treatment and online monitoring of patients on insulin pumps. We offer educational sessions throughout the year in scheduled classes and individual appointments. Our goal is to achieve optimal control of blood sugar in order to avoidn complications resulting from high or low blood sugar levels.
The Insulin Pump Center staff includes our medical director, who is a board certified clinical endocrinologist; a pediatric endocrinologist; nurse pracitioners; registered dietitians; counselors, and certified diabetes educators. All of our staff are certified insulin pump trainers that are well versed in insulin pump therapy. We have certified pump trainers for all recognized pumps and are distinguished as being a center of excellence for insulin pump therapy by the Medtronic Insulin Pump Corporation.
We take pride in our insulin pump program for patients with type 1 and type 2 diabetes. Our goal is to be available to meet our pump patient's needs during and between clinic appointments. Patiens are instruced on how to download their pump at home and forward the download to the clinic for review.
Our staff of diabetes educators, dietitians, nurse practitioners and board certified endocrinologists are well versed with the intricacies of diabetes treatment and mangement using an insulin pump. The team is famililar with and comfortable in prescribing insulin pump therapy as well as monitoring and adjusting insulin pump settings to maintain the patient's diabetes control. We strive to be available to our pump patients during and between clinic appointments.
INSULIN PUMP:
An insulin pump is a small mechanical device which delivers insulin similar to the natural function of the pancreas. The insulin is delivered through a small cannula (tube) that is inserted under the skin into the fat tissue by the user and is changed every 2-3 days.
Rapid acting insulin is used in the pump. The basal rate is a continuous drip of rapid acting insulin replaces the long acting insulin injection. The pump has the capacity to run different basal rates during the day. A bolus insulin dose is usually given at each meal to correct blood sugar and/or cover the carbohydrates consumed. Since the pump only uses rapid acting insulin, it must be worn continuosly.
Are you a good canidate for an Insulin Pump?
If you qualify as far as above requirements are concerned, should consider coming to an introduction to pump class and meet individually with the diabetes educator and review insulin pump therapy for patients who want to experience insulin pump therapy, we have a program where they can use pump for 1-2 weeks to assess the effect of insulin pump therapy on their blood glucose levels as well as therapy related to handle insulin pump therapy before committing to this form of therapy.
What is involved in starting the Pump?
Once the provider/physician/endocrinologist recommends insulin pump therapy to the patients, patients are then assessed on their basic knowledge of diabetes education. They must complete a course of diabetes education as recommended by the American Diabetes Association and come to a pre-pump class. They should also be well versed with carbohydrate-content food and be able to measure the grams of carbohydrate they are consuming. Thereafter a pump is ordered and once approved by the insurance, patients have the pump and they can attend the pump start class.
Once on the pump, patients are required to follow up for their visits, which range every 3-6 months depending on their blood glucose control and the patient using the pump. In addition, patients are also monitored via the Internet if pump therapy needs to be adjusted in between appointments.
What to do if the Insulin Pump fails:
1. Contact the insulin pump company immediately, so better replacement pump can be shift.
2. In the event of failure of the pump, you need to go back to start taking multiple daily injections and have long- and short-acting insulin injections administered.
3. To understand the dose of your therapy contact your healthcare provider if you do not already have the dose that you need.
4. Lantus (inaudible) recovery shortly is 24 hours, so if the pump is started in less than 24 hours of last insulin injection, then a temporary basal may need to be managed to be administered.
5. Sick day.
6. Travel.
7. School.
8. Continuous glucose monitoring system.
We take pride in our insulin pump program for patients with type-I as well as type-II diabetes. Our experience dates back to 1998 when first patient with insulin pump was enrolled in our program.
Our staff of diabetes educators, dieticians, nurse practitioner and physicians who are board certified in endocrinology are well versed with intricacies of treatment of diabetes with insulin pump. The team is familiar and comfortable in prescribing this therapy as well as monitoring and maintaining patient’s care while on the insulin pump.
For the appropriate patient insulin delivery through an insulin pump is closest to the physiologic secretion of insulin via the pancreas. Pump therapy enables the patient to maintain blood glucose close to a “normal” level with significantly less problems with hyper or hypoglycemia in trying to maintain strict blood glucose control.
As proven in the DCCT trial, control of blood glucose level reduces risk of long-term complications related to diabetes. Hence, we believe that prescribing appropriate therapy to achieve tight/strict blood glucose control is in patient’s best interest. Due to our experience with insulin pump therapy for children as well as adults for patients with type-I and type-II diabetes, cystic fibrosis related diabetes and post pancreatectomy diabetes, we are able to provide a comprehensive treatment and monitoring program.
The comprehensive aspect of our care includes a detailed training program. After identifying candidates for insulin pump therapy they are referred to pre-pump session. The patients undergo detailed training to get them familiar with details of pump function, carbohydrate counting. Once patients are ready to start using the pump, they are seen for a "pump start” session, where pump functions are again reviewed in detail and patients get to use the pump hands on, and learn how to put on the pump. After this session patients start to use the pump and are seen in 2-3 days to follow up and to review their first few days of pump therapy, they redo the pump insertion which is supervised to make sure patients are comfortable in this important function. If patients are not comfortable in pump insertion changes, they are seen agin in 2-3 days to redo the post pump session. Once comfortable they are seen at a greater interval for follow up.
Patients are also taught how to upload the pump data online to makes sure pump settings are adequate and do not need adjustment. This adjustment in typically made on follow up visits, however, in order toy keep blood glucose in better control, if we identify patients who need adjustment from their download and they are asked to be seen sooner than their scheduled appointment to get the blood glucose under better control sooner than later.
Our goal is to be available for our patient’s needs to adjust the insulin pump settings in between appointments as a change that may streamline blood glucose levels should not take three months to be done at the next clinic appointments. Hence our experience with online monitoring and counseling is very valuable to our patients.
For those patients who are unsure of adapting this therapy and are suitable candidates, we also offer a trial period where they can try using a pump to see if they will be able to handle insulin delivery through an insulin pump instead of multiple daily injections.
We are experienced in prescribing and monitoring all commercial pumps available in the market and have expertise and experience in the field.
We are distinguished as being designated a center of excellence for insulin pump therapy by Medtronic Incorporation, which is the leading insulin pump manufacturer globally.